Deep brain stimulation parkinsons disease – Deep brain stimulation Parkinson’s disease is a revolutionary treatment for Parkinson’s, offering hope for improved quality of life. This in-depth look explores the intricacies of this procedure, from the underlying neurological mechanisms to the surgical and post-operative considerations. We’ll delve into the various types of electrodes, stimulation parameters, and the intricate process of programming the device, ultimately exploring the potential benefits, risks, and ethical implications of this transformative therapy.
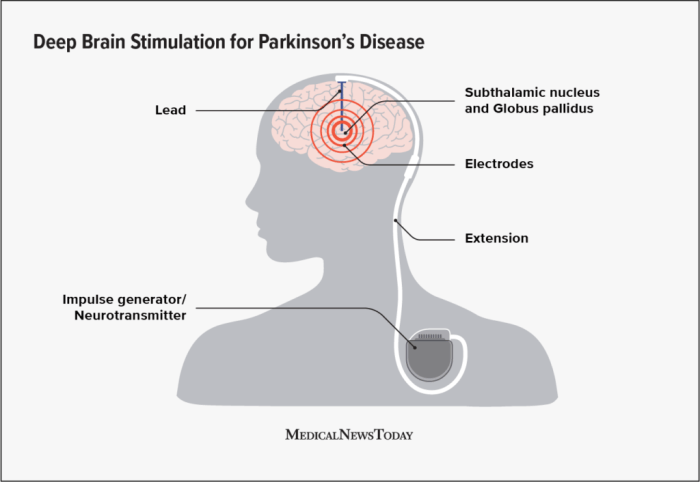
Parkinson’s disease, a debilitating neurodegenerative disorder, manifests through a range of motor symptoms, including tremors, rigidity, and slowness of movement. Deep brain stimulation (DBS) presents a viable surgical option for managing these symptoms. This treatment involves implanting electrodes in specific brain regions, sending electrical impulses to regulate abnormal neuronal activity. This process can lead to significant symptom reduction, improving patients’ overall well-being.
Understanding the nuances of DBS, from the surgical procedure to the long-term effects, is crucial for patients and healthcare providers.
Introduction to Deep Brain Stimulation (DBS) for Parkinson’s Disease
Parkinson’s disease is a progressive neurological disorder affecting movement. Characterized by a gradual decline in motor control, it impacts millions worldwide. Symptoms typically emerge in middle age or later and can include tremors, rigidity, slowness of movement (bradykinesia), and postural instability. These symptoms significantly impair daily activities and quality of life.Deep Brain Stimulation (DBS) is a surgical procedure that involves implanting electrodes in specific brain regions.
These electrodes deliver electrical impulses to modulate abnormal brain activity, potentially alleviating Parkinson’s symptoms. This treatment approach has revolutionized the management of Parkinson’s disease for many patients, offering a way to mitigate the debilitating effects of the condition.
Deep brain stimulation (DBS) for Parkinson’s disease is a fascinating area of research, and it’s amazing how much progress is being made. While exploring the complexities of this treatment, I stumbled across a compelling piece on Marsha P. Johnson’s legacy, specifically focusing on tourmaline. This essay, marsha p johnsons legacy tourmaline essay , offers a fresh perspective on societal issues and resilience.
Ultimately, though, I’m drawn back to the remarkable potential of DBS in alleviating the symptoms of Parkinson’s.
Parkinson’s Disease: A Brief Overview
Parkinson’s disease is primarily characterized by the loss of dopamine-producing neurons in the substantia nigra pars compacta, a crucial brain region. This dopamine deficiency disrupts the intricate balance of neurotransmitters within the basal ganglia, the brain structure responsible for movement control. This disruption directly leads to the motor symptoms that define Parkinson’s. The exact cause of Parkinson’s remains unknown, but genetic predisposition and environmental factors are thought to play a role.
Deep Brain Stimulation (DBS) as a Treatment Option
DBS is a neurosurgical technique used to alleviate symptoms of Parkinson’s disease and other neurological conditions. It involves the precise placement of electrodes within specific brain structures, enabling the delivery of electrical impulses to target areas. These electrical pulses interfere with abnormal neuronal activity, potentially restoring a more normal balance in the brain’s circuitry. The procedure is typically considered when medications fail to adequately control symptoms or when severe side effects from medications emerge.
Historical Context and Development of DBS
The concept of DBS emerged in the mid-20th century, and its application to Parkinson’s disease has evolved significantly over time. Early attempts focused on understanding the role of specific brain regions in movement control. Subsequent research led to the development of advanced electrode technology, surgical techniques, and sophisticated programming methods for optimizing stimulation parameters. These advancements have refined DBS, making it a more precise and effective treatment modality.
Brain Regions Targeted by DBS in Parkinson’s
DBS targets specific brain regions involved in movement control within the basal ganglia. The most common targets are the subthalamic nucleus (STN) and the globus pallidus internus (GPi). The subthalamic nucleus plays a critical role in regulating movement, and stimulating this region can reduce rigidity, tremor, and slowness of movement. The globus pallidus internus is another key structure in the basal ganglia circuit.
Stimulating this region can also improve motor function.
Types of Electrodes Used in DBS Procedures
Various types of electrodes are employed in DBS procedures, each with specific characteristics and potential benefits. These electrodes are designed for long-term implantation and are carefully tailored to the individual patient’s needs. The selection process involves considering factors like the specific target brain region, the patient’s anatomy, and the desired stimulation parameters. They are typically made of insulated materials, such as platinum or iridium, with precise configurations to deliver electrical impulses effectively.
Surgical Procedure and Implantation

Deep brain stimulation (DBS) surgery for Parkinson’s Disease is a complex but potentially life-altering procedure. It involves precisely targeting specific brain regions with electrodes that deliver electrical impulses to alleviate Parkinson’s symptoms. The procedure requires meticulous planning, precise execution, and post-operative care to ensure optimal outcomes. This process will be described in detail, focusing on pre-operative assessments, surgical steps, instrumentation, and post-operative recovery.
Pre-Operative Assessments and Evaluations
Careful pre-operative evaluations are crucial for successful DBS implantation. These assessments determine the suitability of the patient for surgery and help in selecting the optimal stimulation targets. Neurological evaluations assess the extent and nature of Parkinson’s disease symptoms, including motor fluctuations, tremor severity, and non-motor symptoms. These evaluations also include a comprehensive medical history and physical examination to identify any potential contraindications to surgery.
Neuropsychological evaluations are also conducted to assess cognitive function and potential risks associated with the procedure. Imaging studies, such as MRI and CT scans, are used to create detailed anatomical maps of the brain, helping neurosurgeons to precisely locate the target areas for electrode placement.
Surgical Steps Involved in DBS Implantation
The DBS implantation surgery is typically performed under general anesthesia. A craniotomy, a surgical opening in the skull, is made to access the target area in the brain. Precise surgical navigation systems are used to accurately identify the target locations, ensuring that the electrodes are placed in the correct position within the brain. The electrodes are then carefully inserted into the brain using stereotactic techniques, and secured in place.
Electrode placement is often guided by real-time recordings of brain activity, which helps in ensuring optimal stimulation parameters. A small extension wire from the electrodes is connected to a pulse generator (also called a neurostimulator) that is implanted under the skin, usually in the chest area. Finally, the surgical site is closed and monitored post-operatively.
Surgical Setup and Instruments
The surgical setup for DBS implantation is sophisticated and requires specialized equipment. A stereotactic frame is used to accurately position the head during the procedure. High-resolution imaging systems, such as MRI and CT scanners, are used to create detailed 3D images of the brain, allowing for precise targeting. Specialized instruments, such as micro-electrodes and manipulators, are used for precise electrode placement.
The neurosurgical team uses advanced surgical navigation systems that provide real-time guidance and allow the surgeon to precisely control the depth and location of electrode placement.
Deep brain stimulation (DBS) for Parkinson’s disease is a fascinating area of medical research. It’s all about precisely targeting specific brain regions to alleviate symptoms. Recently, the US and UK have been in the news regarding trade deals, with Trump and Starmer involved in negotiations, affecting tariffs and agreements. This recent trade agreement highlights the complex interplay between global economic forces and even the advancement of medical procedures like DBS.
It’s remarkable how the latest news about global trade dynamics can still influence our understanding of this groundbreaking medical treatment for Parkinson’s disease.
Post-Operative Care and Recovery
Post-operative care is crucial for a smooth recovery. Patients are monitored closely for any complications, such as bleeding, infection, or seizures. Pain management and medication adherence are vital to ensure patient comfort and well-being. Physical therapy and speech therapy are often recommended to help patients regain lost motor skills and improve communication. Regular follow-up appointments are scheduled to adjust stimulation parameters and monitor the effectiveness of the treatment.
Patients are educated about potential side effects, how to manage them, and the importance of regular check-ups.
Comparison of DBS Electrode Models
| Electrode Model | Electrode Configuration | Lead Length | Number of Contacts | Applications |
|---|---|---|---|---|
| Medtronic 3389 | Quadripolar | Variable | 4 | Parkinson’s disease, Essential tremor |
| St. Jude Medical 3389 | Quadripolar | Variable | 4 | Parkinson’s disease, Essential tremor |
| Boston Scientific | Variable | Variable | Variable | Parkinson’s disease, Dystonia |
The table above provides a simplified comparison of DBS electrode models. Each model has specific configurations, lengths, contact numbers, and applications, tailored to different patient needs and surgical scenarios. It is important to note that electrode selection is a collaborative process between the patient, neurosurgeon, and neurologist.
Stimulation Parameters and Programming
Deep brain stimulation (DBS) for Parkinson’s Disease isn’t a one-size-fits-all treatment. The effectiveness of DBS hinges critically on precise programming of the stimulation parameters. This intricate process allows neurologists and neurosurgeons to tailor the stimulation to the individual patient’s needs, optimizing symptom relief while minimizing side effects. Each patient’s response to stimulation is unique, necessitating careful adjustment of various parameters.Precise control over stimulation is paramount to achieving the best possible outcome for Parkinson’s patients.
By adjusting these parameters, clinicians can fine-tune the delivery of electrical pulses to specific brain regions, thereby mitigating the debilitating motor symptoms associated with Parkinson’s. Careful programming requires expertise in both neurology and neurosurgery, ensuring that stimulation is effective and well-tolerated.
Adjustable Stimulation Parameters
The DBS system allows for adjustments in several crucial parameters. These adjustments are meticulously performed to maximize therapeutic benefit while minimizing side effects. Understanding these parameters is essential to comprehending the intricate process of DBS programming.
- Pulse Width: This parameter dictates the duration of each electrical pulse delivered to the target brain region. A shorter pulse width generally results in less discomfort for the patient. However, insufficient pulse width may not effectively stimulate the targeted neurons, potentially limiting symptom relief. Adjustments are made based on the patient’s individual response, ensuring optimal efficacy and tolerability.
- Pulse Frequency: This parameter refers to the number of electrical pulses delivered per second. Higher frequencies can sometimes lead to greater symptom improvement, but may also increase the risk of side effects. The optimal frequency is determined through careful monitoring of the patient’s response and adjusting the stimulation parameters accordingly.
- Stimulation Amplitude: This parameter controls the strength of the electrical current delivered. Increasing the amplitude can sometimes improve symptom relief, but excessive stimulation can induce adverse effects. Therefore, precise control of the stimulation amplitude is essential to maximize efficacy and minimize discomfort.
- Pulse Train Duration: This parameter defines the duration for which the pulses are delivered in a series. A longer pulse train duration generally allows for more sustained stimulation of the target area, but may also result in greater stimulation-related side effects. The optimal pulse train duration is individually determined based on the patient’s response and tolerance.
Programming the DBS Device
DBS device programming is a dynamic process, not a one-time event. The process involves careful observation and adjustment of stimulation parameters to optimize therapeutic efficacy and patient comfort.
- Initial Programming: Initial programming often takes place in a specialized clinic or hospital immediately following the implantation procedure. The neurologist and neurosurgeon work together to establish a baseline stimulation protocol. This initial setup serves as a foundation for subsequent adjustments.
- Follow-up Programming: Ongoing follow-up appointments are crucial for fine-tuning the stimulation parameters. Neurologists and neurosurgeons evaluate the patient’s response to stimulation, making adjustments as needed. The goal is to optimize symptom relief while minimizing side effects.
- Neurologist’s Role: The neurologist plays a critical role in assessing the patient’s symptoms and neurological status. They monitor the effects of the stimulation on motor function, balance, and other symptoms related to Parkinson’s disease. The neurologist works closely with the neurosurgeon to optimize the stimulation parameters.
- Neurosurgeon’s Role: The neurosurgeon provides crucial insights into the location and function of the implanted electrodes. They are responsible for confirming the accuracy of electrode placement and can help determine the optimal stimulation parameters for a particular patient. Neurosurgeons also contribute to the patient’s overall care, especially in the initial programming phase.
Stimulation Waveforms
Various stimulation waveforms are available, each with its own characteristics and potential benefits.
- Monophasic Stimulation: This type of stimulation involves a single pulse delivered to the target region. It is a simple form of stimulation, but it may not provide the most effective symptom relief for all patients.
- Biphasic Stimulation: This type of stimulation involves two pulses of opposite polarity, delivered sequentially. This method is often more effective in reducing side effects and improving symptom control.
Comparison of Stimulation Parameters
| Parameter | Description | Effect on Symptoms |
|---|---|---|
| Pulse Width | Duration of each electrical pulse | Shorter pulses generally lead to less discomfort; longer pulses may be necessary for effective symptom control. |
| Pulse Frequency | Number of pulses per second | Higher frequencies may provide better symptom relief but can increase side effects. |
| Stimulation Amplitude | Strength of the electrical current | Higher amplitudes can improve symptoms, but excessive stimulation can cause discomfort or side effects. |
| Pulse Train Duration | Duration for which pulses are delivered in a series | Longer pulse trains may offer sustained symptom relief but can increase side effects. |
Benefits and Limitations of DBS
Deep Brain Stimulation (DBS) offers a transformative approach to managing Parkinson’s Disease symptoms, but like any medical intervention, it comes with its own set of advantages and disadvantages. Understanding these aspects is crucial for patients and their families in making informed decisions about this treatment option. DBS is not a cure for Parkinson’s, but it can significantly improve quality of life for many individuals.DBS aims to modulate specific brain regions to reduce motor symptoms, enabling patients to regain some lost functionality and independence.
However, the procedure is invasive, and long-term effects can vary. Understanding the nuances of both benefits and limitations is vital for a realistic expectation of the therapy’s potential impact.
Potential Benefits of DBS, Deep brain stimulation parkinsons disease
DBS can dramatically alleviate the debilitating motor symptoms of Parkinson’s, such as tremors, rigidity, slowness of movement (bradykinesia), and postural instability. Many patients report a significant improvement in their ability to perform daily tasks, leading to increased independence and improved quality of life. These improvements are often noticeable, and can be significant enough to allow patients to return to activities they had previously been unable to participate in, like gardening or playing a musical instrument.
Reduced medication needs are another important benefit, as DBS can lessen the side effects associated with high doses of Parkinson’s medication.
Potential Long-Term Effects of DBS
The long-term effects of DBS are multifaceted. While the initial improvements are often sustained, some patients may experience a gradual decline in efficacy over time. Factors like the progression of Parkinson’s itself, the specific stimulation parameters, and individual patient responses can all influence these long-term outcomes. Regular follow-up appointments and adjustments to the stimulation parameters are crucial to maintaining optimal results.
Long-term follow-up studies are vital to understanding the evolving impact of DBS on patients.
Potential Risks and Complications of DBS
DBS, like any surgical procedure, carries potential risks and complications. These may include infection, bleeding, stroke, and damage to surrounding brain tissues. Furthermore, there’s a possibility of hardware malfunction or lead displacement. The potential for side effects from stimulation parameters also exists. These complications are generally rare but can be serious.
Thorough pre-operative evaluation and careful surgical technique are essential to minimize these risks. Patients should be well-informed about the possible side effects and complications.
Comparison of DBS with Other Treatment Options
Medication remains the cornerstone of Parkinson’s treatment. However, as Parkinson’s progresses, medication alone may become insufficient to manage symptoms effectively. Deep brain stimulation offers an alternative approach for those who have not responded adequately to medication or experience unacceptable side effects. Surgical options like pallidotomy and thalamotomy are less common today and are often compared to DBS.
Each treatment has its own set of benefits and limitations, and the most suitable option depends on the individual patient’s specific needs and circumstances.
Comparison Table: DBS vs. Medications for Parkinson’s
| Feature | Medications | DBS |
|---|---|---|
| Mechanism of Action | Mimics or replaces dopamine in the brain. | Stimulates specific brain regions to reduce abnormal neuronal activity. |
| Symptom Management | Effective for early-stage symptoms but may lose effectiveness over time. | Effective for managing a wider range of symptoms, particularly in later stages, and can provide sustained relief. |
| Side Effects | Potential for nausea, vomiting, sleep disturbances, and involuntary movements (dyskinesias). | Potential for infection, bleeding, stroke, hardware malfunction, and stimulation-related side effects. |
| Long-Term Efficacy | Usually requires frequent adjustments as the disease progresses. | Potentially sustained relief, though adjustments may be needed. |
| Cost | Generally lower initial cost, but long-term costs can accumulate with frequent adjustments and follow-up care. | Higher initial cost due to surgical procedures and device implantation, but potential for long-term cost savings through reduced medication needs. |
Patient Selection and Outcomes
Deep brain stimulation (DBS) for Parkinson’s Disease offers a transformative approach to symptom management, but it’s not a one-size-fits-all solution. Careful patient selection is crucial to maximizing the benefits and minimizing potential complications. This section delves into the criteria for choosing suitable candidates, factors impacting treatment success, and real-world examples illustrating the profound impact DBS can have on quality of life.Understanding the nuances of patient selection and potential outcomes empowers both patients and healthcare providers to make informed decisions about this complex procedure.
Factors such as disease severity, medication responsiveness, and the patient’s overall health profile play a critical role in determining the appropriateness of DBS.
Patient Selection Criteria
Careful evaluation is essential to identify patients who are most likely to experience significant benefits from DBS. The process typically involves a multidisciplinary team approach, incorporating neurological assessments, cognitive testing, and psychosocial evaluations. Patients should exhibit a significant and persistent response to medication, but this response must be inadequate to control their symptoms.
- Motor Fluctuations and Dyskinesias: Patients experiencing significant motor fluctuations (on-off phenomenon) and disabling dyskinesias (involuntary movements) are often strong candidates. These symptoms often become progressively difficult to manage with medication alone.
- Non-Motor Symptoms: The presence of non-motor symptoms, such as sleep disturbances, depression, or cognitive impairment, should be carefully considered. DBS may potentially alleviate some of these symptoms, although the extent of improvement varies.
- Disease Duration and Progression: The duration and progression of Parkinson’s Disease are important factors. Patients with moderate to severe disease, but without significant cognitive decline, are generally considered good candidates.
- Medical History and Co-morbidities: Pre-existing medical conditions, such as cardiac issues or psychiatric disorders, require careful consideration. A comprehensive medical history is crucial to identify potential risks and tailor the DBS procedure accordingly.
- Cognitive Function and Mental Status: Cognitive function and mental status are assessed thoroughly. Patients with preserved cognitive abilities and stable mental health are more likely to benefit from DBS.
Factors Influencing DBS Success
Several factors can influence the success of DBS therapy. These include surgical precision, electrode placement, stimulation parameters, and the patient’s active participation in post-operative rehabilitation.
- Surgical Technique and Electrode Placement: Accurate targeting of the specific brain regions affected by Parkinson’s Disease is paramount. Minimally invasive surgical techniques and advanced imaging guidance play a crucial role.
- Stimulation Parameter Optimization: Precise adjustment of stimulation parameters is essential. Individualized programming is critical to maximize symptom relief while minimizing side effects. This is a dynamic process, requiring follow-up appointments to refine the stimulation.
- Patient Compliance and Engagement: Patient cooperation and active participation in post-operative follow-up and rehabilitation are crucial. Regular follow-up visits, adjustments to stimulation parameters, and compliance with lifestyle recommendations all contribute to the long-term effectiveness of DBS.
Patient Experiences with DBS
Numerous patients have reported significant improvements in their quality of life following DBS. These improvements often include reduced tremor, improved motor function, and a decrease in medication-related side effects.
“I was so exhausted from the constant tremor and stiffness. DBS has given me back my life. I can now walk and participate in activities I haven’t been able to do in years.”
John Smith, DBS Patient
Impact on Quality of Life
DBS can profoundly improve patients’ quality of life by alleviating debilitating symptoms and enabling greater independence. Patients often report improved mobility, reduced anxiety, and a return to hobbies and social activities they had previously abandoned.
Patient Selection Criteria Table
| Criterion | Description | Importance |
|---|---|---|
| Motor Fluctuations | Significant on-off phenomenon | Strong indicator of potential benefit |
| Dyskinesias | Severe involuntary movements | Potential for significant improvement |
| Non-Motor Symptoms | Sleep disturbances, depression, etc. | Assess potential for improvement with DBS |
| Disease Duration | Duration of Parkinson’s | Important factor in candidate evaluation |
| Medical History | Pre-existing medical conditions | Critical for risk assessment |
| Cognitive Function | Cognitive ability assessment | Essential to evaluate suitability |
Future Directions and Research
Deep brain stimulation (DBS) for Parkinson’s disease has shown remarkable success, but ongoing research continues to refine and expand its application. Researchers are exploring new avenues to optimize stimulation protocols, improve patient selection, and even extend the benefits of DBS to other neurological disorders. The future of DBS promises exciting advancements that could significantly improve the lives of those affected by these debilitating conditions.
Deep brain stimulation for Parkinson’s disease offers promising treatments, but access to advanced medical care isn’t universal. Consider the struggles faced by patients in Burundi, where limited resources impact treatment options. For instance, exploring the role of US foreign aid in supporting healthcare initiatives for Burundian patients with neurological conditions like Parkinson’s is crucial, as detailed in this insightful essay on US foreign aid Burundi patients essay.
Ultimately, ensuring equitable access to life-changing treatments like deep brain stimulation remains a global challenge.
Advanced Stimulation Techniques
Researchers are constantly developing more sophisticated stimulation strategies. These advancements aim to tailor stimulation parameters to individual patient needs and to minimize side effects. Closed-loop stimulation, a cutting-edge technique, adjusts stimulation intensity in real-time based on the patient’s neural activity. This dynamic approach allows for more precise and targeted treatment, potentially reducing the side effects often associated with traditional DBS.
Furthermore, incorporating brain imaging and machine learning algorithms into the stimulation process can optimize outcomes by adapting to subtle changes in the patient’s condition.
Targeting New Neural Pathways
Beyond the established targets, researchers are investigating other neural pathways that might influence motor control and non-motor symptoms in Parkinson’s disease. This exploration could lead to the development of new stimulation targets, offering more comprehensive relief from the diverse symptoms associated with the condition. For instance, future studies might explore targeting areas implicated in cognitive function or sleep disturbances.
This approach could significantly improve the quality of life for Parkinson’s patients by addressing a broader spectrum of their symptoms.
DBS for Other Neurological Disorders
The potential of DBS extends beyond Parkinson’s disease. Studies are underway to evaluate its effectiveness in treating other neurological conditions such as essential tremor, dystonia, and obsessive-compulsive disorder. Preliminary results are promising, suggesting that DBS could offer a viable therapeutic option for these disorders as well. The key lies in understanding the specific neural circuits involved in each disorder and tailoring the stimulation parameters to those circuits.
Ongoing Research in Parkinson’s Disease DBS
Several key areas of research focus on improving the efficacy and safety of DBS for Parkinson’s. These investigations are addressing areas like:
- Predictive Modeling for Optimal Patient Selection: Developing algorithms to predict patient response to DBS based on various factors, including demographics, disease characteristics, and pre-operative assessments, allows for better patient selection, enhancing the chances of positive outcomes and reducing the likelihood of adverse effects.
- Personalized Stimulation Parameters: Tailoring stimulation parameters to individual patient needs through real-time adjustments based on neural activity and symptom severity. This personalized approach aims to maximize therapeutic benefits while minimizing side effects.
- Minimally Invasive Techniques: Developing new, less invasive methods for DBS implantation, such as smaller electrodes or less disruptive surgical approaches, could lead to improved patient recovery and reduced post-operative complications.
- Long-Term Effects and Maintenance: Investigating the long-term effects of DBS on the brain and developing strategies for maintaining optimal stimulation parameters over time are crucial for maximizing the longevity and effectiveness of the treatment.
Emerging Research Areas in DBS for Parkinson’s
| Research Area | Description |
|---|---|
| Closed-Loop DBS | Real-time adjustment of stimulation parameters based on neural activity and patient feedback. |
| Deep Brain Stimulation and Cognitive Function | Investigating the impact of DBS on cognitive functions, such as memory and executive function, in Parkinson’s patients. |
| DBS for Non-Motor Symptoms | Evaluating the potential of DBS to alleviate non-motor symptoms of Parkinson’s, such as sleep disturbances, depression, and anxiety. |
| Combination Therapies | Exploring the potential benefits of combining DBS with other therapies, such as medication or physical therapy, to enhance treatment outcomes. |
| Predictive Modeling for Optimal Patient Selection | Developing algorithms to predict patient response to DBS based on various factors, including demographics, disease characteristics, and pre-operative assessments. |
Ethical Considerations
Deep brain stimulation (DBS) for Parkinson’s disease presents a complex interplay of medical benefits and ethical considerations. While offering significant potential for symptom relief, the procedure raises important questions about patient autonomy, informed consent, and the potential for unintended consequences. Navigating these ethical complexities is crucial for ensuring responsible and equitable access to this potentially life-altering treatment.The ethical landscape surrounding DBS requires careful consideration of the patient’s rights, potential risks, and the broader societal implications.
Balancing the potential benefits of symptom reduction with the inherent risks of invasive surgery and the possibility of unforeseen complications necessitates a robust ethical framework. This framework must be applied consistently across diverse patient populations, while also adapting to evolving scientific understanding and technological advancements.
Informed Consent and Patient Autonomy
A cornerstone of ethical DBS practice is the principle of informed consent. Patients undergoing DBS must fully comprehend the procedure’s risks, benefits, alternatives, and potential long-term consequences. This includes not only the physical risks, but also the potential psychological and social impacts. Explaining the procedure in a manner that is both accessible and comprehensive is essential for empowering patients to make informed decisions.
Detailed and understandable information materials, presented in multiple formats, can enhance the patient’s understanding. A clear and comprehensive description of the risks, benefits, and alternatives should be provided in a manner that is easily understandable and avoids overly technical jargon.
Patient Well-being and Potential Risks
Patient well-being is paramount in DBS. The procedure itself carries risks, including infection, bleeding, stroke, and damage to surrounding brain tissue. Beyond physical risks, there’s the potential for psychological side effects, such as mood changes, cognitive impairment, or personality shifts. It is crucial to establish robust post-operative monitoring and support systems to address these potential complications. The ethical obligation extends beyond the immediate surgical procedure to encompass ongoing care and support, addressing both physical and psychological needs.
Detailed monitoring protocols should be in place, including regular follow-up appointments and psychological assessments, to identify and manage any emerging problems.
Ethical Dilemmas in DBS
Ethical dilemmas in DBS can arise in various contexts. One significant dilemma involves selecting patients for the procedure. Criteria for patient selection must be transparent and equitable, avoiding bias based on socioeconomic status, ethnicity, or access to healthcare. Another dilemma concerns the potential for overtreatment or undertreatment, where the fine-tuning of stimulation parameters necessitates careful consideration of individual patient needs and preferences.
Careful consideration of patient preferences, along with a rigorous risk-benefit analysis, is crucial in navigating these complex situations.
Ethical Principles in DBS
| Ethical Principle | Considerations in DBS |
|---|---|
| Beneficence | Maximizing benefits and minimizing harm for the patient. This includes careful selection of patients, meticulous surgical technique, and ongoing monitoring for complications. |
| Non-maleficence | Avoiding harm or minimizing potential risks associated with the procedure. This includes thorough risk assessment, informed consent procedures, and ongoing management of complications. |
| Autonomy | Respecting patient’s right to make informed decisions regarding their treatment. This involves providing comprehensive information about the procedure, its potential benefits and risks, and alternative treatment options. |
| Justice | Ensuring equitable access to DBS, considering factors like socioeconomic status, geographic location, and insurance coverage. |
| Respect for Persons | Treating patients with dignity and respect, acknowledging their vulnerability, and empowering them to actively participate in their care. |
Closing Notes: Deep Brain Stimulation Parkinsons Disease
In conclusion, deep brain stimulation for Parkinson’s disease offers a promising avenue for symptom management, but it’s crucial to weigh the benefits against potential risks and complications. Patient selection, meticulous surgical precision, and careful programming of stimulation parameters are essential for optimizing outcomes. As research continues to advance, the future of DBS holds the potential for even more effective and targeted treatments, paving the way for a brighter future for Parkinson’s patients.

